Creating a range of resources to support the work of Champions and Practitioners.
Alcohol can also contain lots of calories (kcal) and should be limited to no more than 14 units a week for men and women.
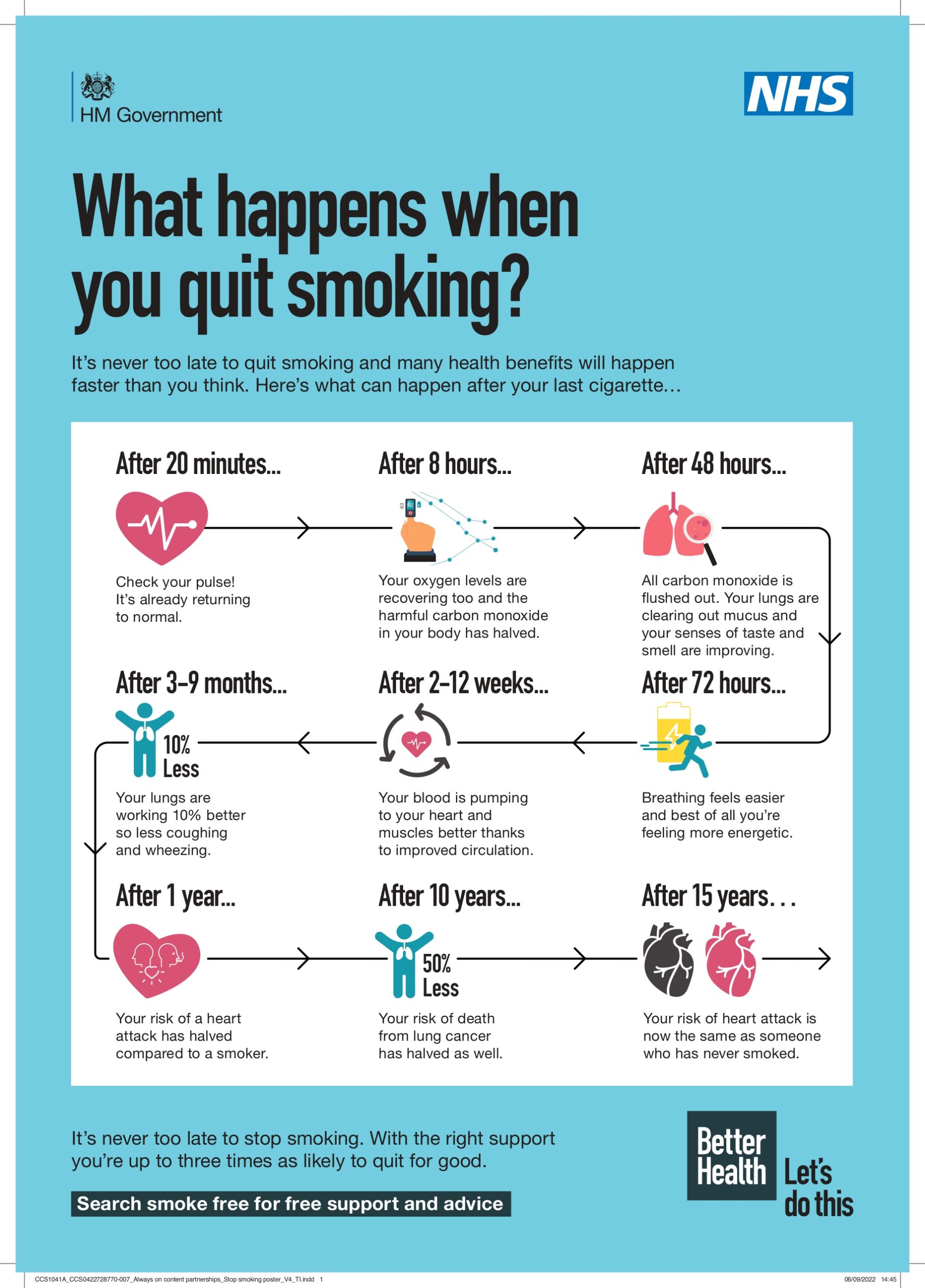
The calorific content of an alcoholic beverage depends on the type of alcohol, the volume served and the addition of mixers. As an example, 1 pint of standard strength lager contains approximately 136kcal, a 175ml medium glass of wine contains approximately 135kcal and a 25ml shot of spirit (40% vol) contains approximately 56kcal.Smoking is the single greatest preventable cause of death in the world today. There are more than one billion smokers worldwide – that’s one quarter of all adults – and it’s killing up to half the people who smoke. (NHS)
For more information on alcohol, see Alcohol: applying All Our Health
There is an interactive e-learning version of this topic now available by NHS.
Drinkaware is the UK’s leading alcohol charity. Working together with individuals, communities, academics, researchers, industry and governments, they have a vision of reducing alcohol harm in the UK

Alcohol misuse, sometimes also known as substance abuse, is when someone’s drinking becomes problematic, harmful, or dependent.
By ‘problematic, harmful, or dependent’ we mean when someone is:
Cancer is when abnormal cells divide in an uncontrolled way. Some cancers may eventually spread into other tissues. There are over 200 different types of cancer.
We do not know all of the causes of cancer, but we do know about the possible risk factors that can affect the chances of developing cancer.
What is cancer? (BSL enabled) | Macmillan Cancer Support – YouTube
Find out more information here
Common symptoms of cancer:
Lifestyle changes to try and reduce the risk of cancer:
Cancer screening is for people without symptoms. It uses tests to find people who may:
Diagnosing cancer early can mean treatment is more effective and less complex. The earlier a cancer is diagnosed, the better your chance of survival and being cured.
There are 3 national cancer screening programmes in the UK:
Bowel cancer screening, is offered to people starting from the age of 50-60 up to 74 in England and Wales. In Northern Ireland it’s offered to people aged 60-74. In Scotland people aged 50-74 are offered bowel cancer screening.
Breast cancer screening is offered to women (including some transgender women), some transgender men and some non-binary people aged 50-70 in the UK.
Cervical screening is offered to women, some transgender men and some non-binary people aged 25-64 in the UK.
Find out more information here
Screening for other cancers: Seek your GP if you have any concerns that you may have other cancer that is not part of the three national programmes.
Should you have any concerns between the screening intervals or you are not within the age groups of the national screening programmes, contact your GP.
In Your Area is an online directory of cancer support services, self-help and support groups, and fundraising events across the UK.
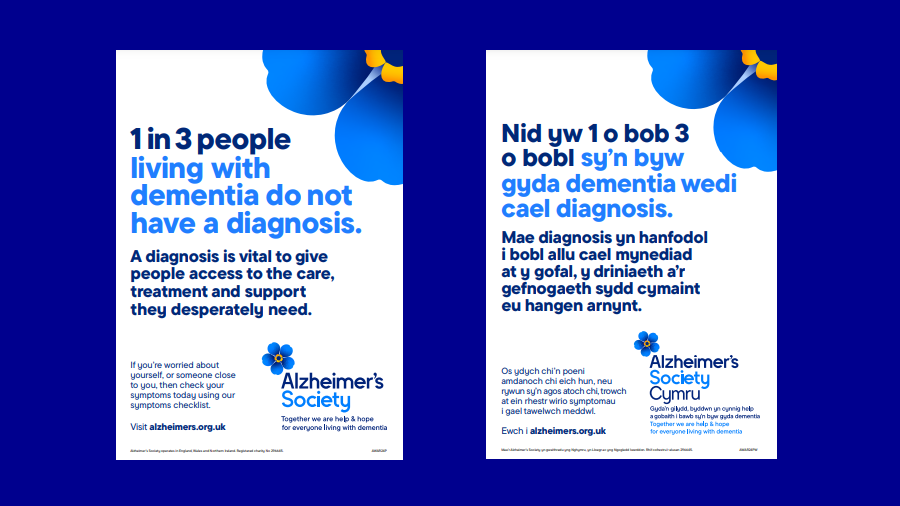
Alzheimer’s disease is the most common cause of dementia in the UK.
Dementia is the name for a group of symptoms associated with an ongoing decline of brain functioning. It can affect memory, thinking skills and other mental abilities.
The exact cause of Alzheimer’s disease is not yet fully understood, although a number of things are thought to increase your risk of developing the condition.
These include:
As the condition develops, memory problems become more severe and further symptoms can develop, such as:
Your local authority has a duty to do a care and support needs assessment to find out what help you need.
A care and support needs assessment is free.
You can apply for a needs assessment by social services on GOV.UK. Alternatively, a GP, consultant, or another health or social care professional can make a referral to your local authority, after getting your consent.
For more information, read the Alzheimer’s Society’s guide to care and support in England.
Getting a Diagnosis for Alzheimer’s
Read more about what to do if you have just been diagnosed with dementia
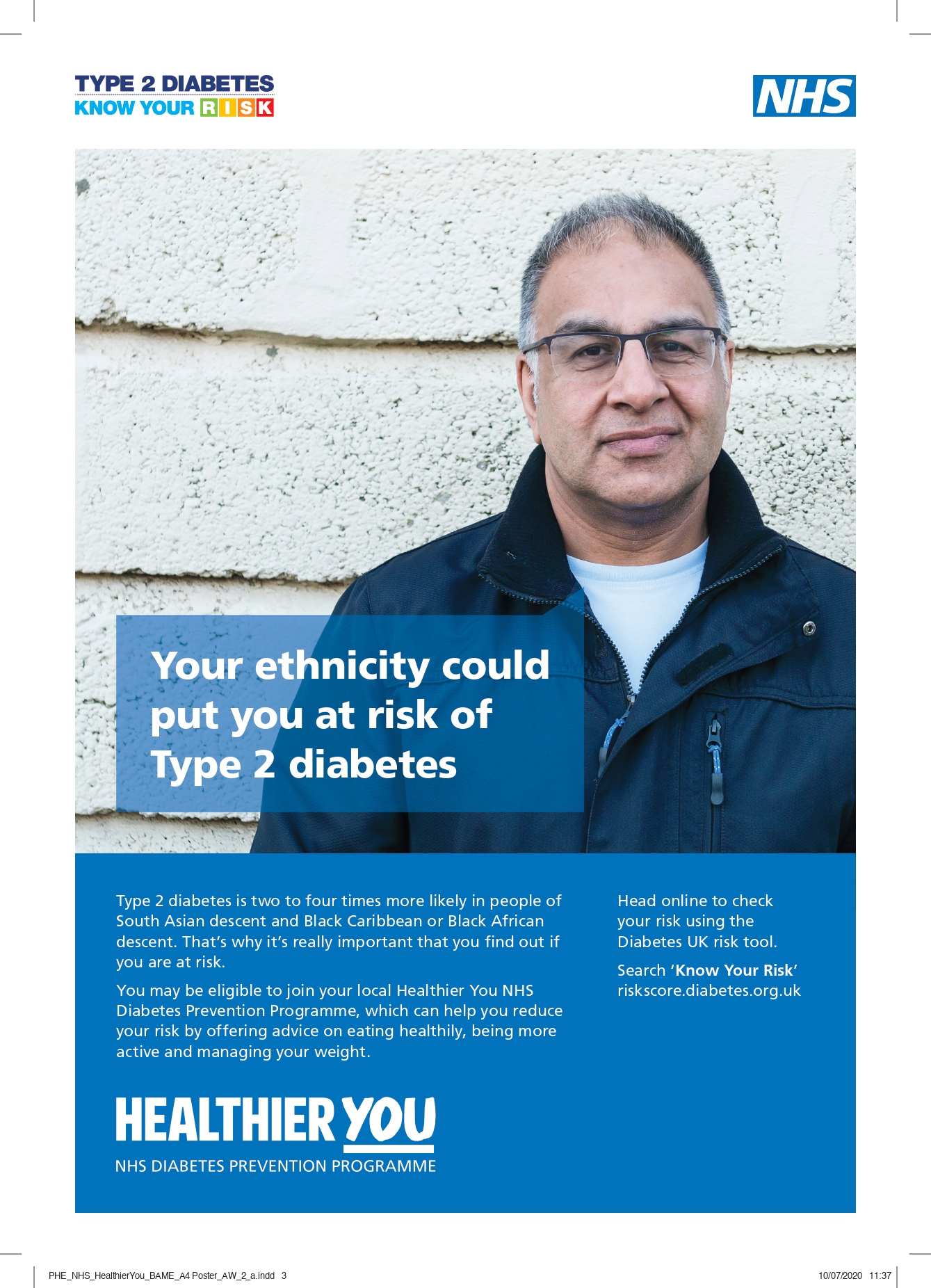
Diabetes is a chronic disease that occurs either when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. Insulin is a hormone that regulates blood glucose. Hyperglycaemia, also called raised blood glucose or raised blood sugar, is a common effect of uncontrolled diabetes and over time leads to serious damage to many of the body’s systems, especially the nerves and blood vessels. ( World Health Organisation)
Find out more on the Diabetes UK website
Support people with diabetes, and those at risk of developing type 2 diabetes to live their lives to the full in North West London.
Find out if you’re at risk of developing type 2 diabetes through this quiz
Please be aware, the results might not be completely accurate if you have any pre-existing health conditions.
Government advice on a healthy, balanced diet is encapsulated in the UK’s national food model, the Eatwell Guide. The Eatwell Guide reflects the latest dietary recommendations and key public health messages. It applies to most people over the age of 5 and is suitable for vegans and vegetarians too.
The food group segment sizes of the Eatwell Guide were developed objectively using a mathematical modelling approach, underpinned by the scientific evidence base. This resulted in a model that meets UK dietary recommendations.
The proportions shown are representative of food consumption over the period of a day or even a week, not necessarily each mealtime.
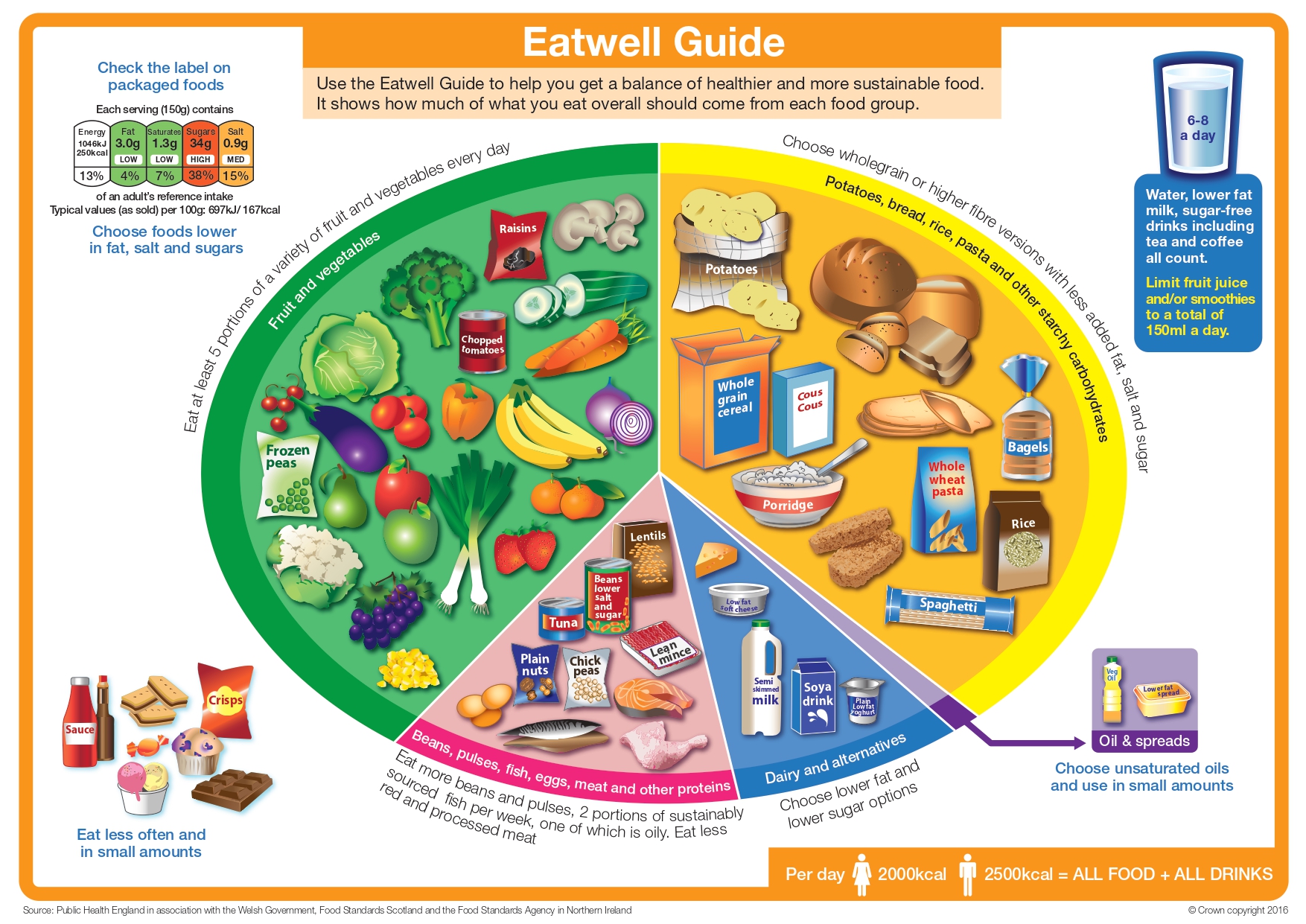
The Eatwell Guide provides a visual representation of the types and proportions of foods needed for a healthy balanced diet to promote long-term health at a population level and includes key messages such as:
The Eatwell Guide principles apply to most people regardless of weight, dietary restrictions, dietary preferences or ethnic origin. The foods included in the image are recognised as representative of the wider food group, including foods specific to particular ethnic minority groups.
The Freshwell Low Carb Project is an initiative set up by Dr David Oliver and Dr Kim Andrews at the Freshwell Health Centre, Essex, UK, to encourage the members of its community to live a Real Food Low Carb lifestyle, so they may be as healthy as possible.
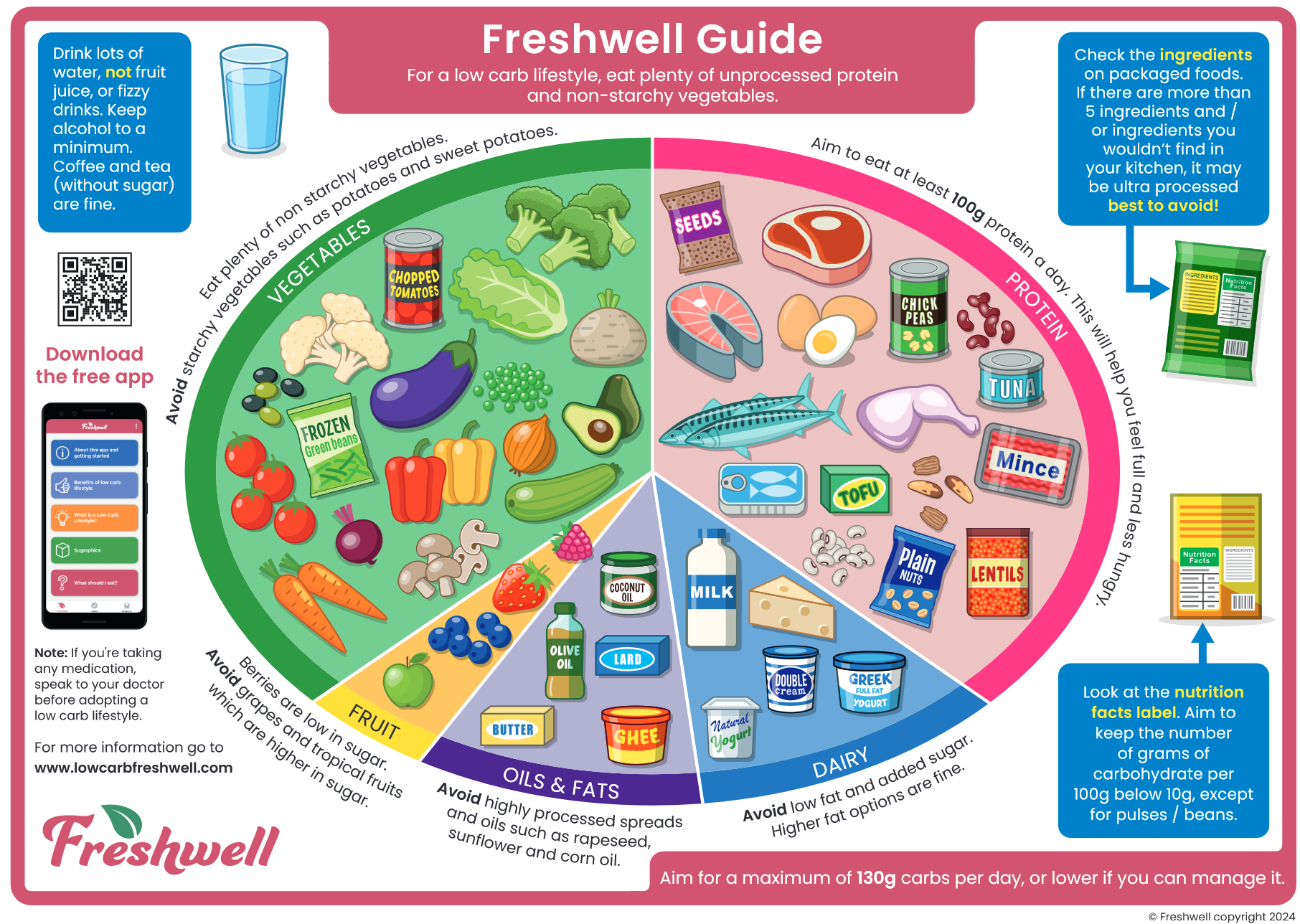
More information about the Freshwell Guide can be found here.
Everyone should aim to drink 6 to 8 glasses of fluid every day. Water, lower fat milk and sugar-free drinks including tea and coffee all count. Although drinks containing caffeine, such as tea and coffee, are mild diuretics, the fluid component of these (for example, water and milk) negates any dehydrating effect at normal levels of consumption.
Fruit juices and smoothies also count towards fluid consumption, although they should be limited to no more than a combined total of 150ml a day.
Sugary drinks are one of the main contributors to excess sugar consumption amongst children and adults in the UK. Swap sugary soft drinks for diet, sugar-free or no added sugar varieties to reduce sugar intake in a simple step.
More information on hydration can be found here

Physical inactivity is associated with 1 in 6 deaths in the UK and is estimated to cost the UK £7.4 billion annually (including £0.9 billion to the NHS alone). Unfortunately, our population is around 20% less active than in the 1960s. If current trends continue, it will be 35% less active by 2030. Many people don’t realise that physical activity has significant benefits for health, both physical and mental, and can help to prevent and manage over 20 chronic conditions and diseases, including some cancers, heart disease, type 2 diabetes and depression.
How to stay active and feel great in Harrow
Statistics related to obesity can be found here
Physical activity guideline can be found here
Quiz on which physical activity suits you by the British Heart Foundation



There are ways you can reduce your risk of having a fall, including making simple changes to your home and doing exercises to improve your strength and balance.
If you have fallen in the past, making changes to reduce your chances of having a fall can also help you overcome any fear of falling.
Some older people may be reluctant to seek help and advice from a GP and other support services about preventing falls because they believe their concerns will not be taken seriously.
But all healthcare professionals take falls in older people very seriously because of the significant impact they can have on a person’s health.
Discuss any falls you have had with a GP and say if it’s had any impact on your health and wellbeing.
The GP can carry out some simple balance tests to check whether you’re at an increased risk of falling in the future. They can also refer you to useful services in your local area.
Tips for preventing falls in the home include:
Doing regular strength exercises and balance exercises can improve your strength and balance, and reduce your risk of having a fall.
This can take the form of simple activities such as walking and dancing, or specialist training programmes.
Many community centres and local gyms offer specialist training programmes for older people.
Exercises that can be carried out at home are also available. Ask a GP about training programmes in your area.
It’s important that a strength and balance training programme is tailored to the individual and monitored by an appropriately trained professional.
There’s also evidence that taking part in regular tai chi sessions can reduce the risk of falls. Tai chi is a Chinese martial art that places particular emphasis on movement, balance and co-ordination.
Unlike other martial arts, tai chi does not involve physical contact or rapid physical movements, making it an ideal activity for older people.
Look after your eyes and make an appointment to have a sight test if you’re concerned that vision loss (even when wearing glasses) is increasing your risk of having a fall.
Not all vision problems can be cured, but some problems can be treated with surgery – for example, cataracts can be removed using cataract surgery.
Drinking alcohol can lead to loss of co-ordination and exaggerate the effects of some medicines.
This can significantly increase the risk of a fall, particularly in older people.
Avoiding alcohol or reducing the amount you drink can reduce your risk of having a fall.
Excessive drinking can also contribute to the development of osteoporosis.
The first 1001 days (from conception to age 2) are recognised as a crucial period during which the foundations for future health and wellbeing are built. Positive experiences – and good quality parent-infant relationships during this time – are associated with the formation of a secure attachment which contributes to good physical and mental health, speech and language development, emotional self-regulation, resilience and wider social and economic
advantages throughout the life course
The Health profile for England, which indicates that overall child health in England has continued to improve.
However, children who live in more deprived areas were more likely to:
Health inequalities are seen across all indicators presented. Health inequalities are not inevitable and can be significantly reduced; however, focusing solely on the most disadvantaged will not reduce health inequalities sufficiently.
To reduce the steepness of the social gradient in health, actions must be universal, but with a scale and intensity that is proportionate to the level of disadvantage. Marmot (2010) (PDF, 16.2MB)
All Our Health takes an ecological approach to improve outcomes for children by addressing the child as an individual within the context of his or her family, community and the wider system in which children and families live.

The Family Hubs are located across Harrow and provide a wide range of free services and classes to support local children and young people and their families. Sessions include breastfeeding support and Learning through Play.
Breastfeeding is an important public health priority. Supporting families to breastfeed and increasing the number of babies who are breastfed gives babies the best possible start.
Breastfeeding improves infant and maternal health and wellbeing in both the short and longer term and research demonstrate:
Breastfeeding can be protective against obesity, particularly in those who are genetically predisposed; breastfeeding for 3 months in the first year of a baby’s life reduces the risk of obesity by 13% in later life. Additionally, mothers who breastfeed benefit from a faster return to pre-pregnancy weight.
Early years high impact supports breastfeeding initiation and maintenance with links to evidence and resources.
Reducing unintentional injuries in childhood remains an important public health priority. Unintentional injuries in and around the home are a leading cause of preventable death for children under 5 years and are a major cause of ill health and serious disability. The majority of unintentional injuries are preventable and they disproportionately affect children living in socioeconomic disadvantage.
Even when local authorities have child injury rates that are similar to those for England, this may mask significant inequalities between smaller geographical areas (districts, wards) within local authorities which need addressing. Local authorities should consider not only the overall child injury rate but also the extent of inequalities in child injury rates across smaller geographical areas when deciding what child injury prevention actions are required.
Data analysis shows that the emergency hospital admission rate for unintentional injuries among the under 5s is 42% higher for children from the most deprived areas compared with children from the least deprived, and for some injury types this inequality may be much larger. These inequalities support the targeting of preventative interventions to children and young people living in the most deprived areas.
Early years high impact area 5 promotes health literacy, accident prevention and the management of minor illnesses with links to evidence and resources.
Read more about reducing unintentional injuries in children under 5
A number of resources have been published to support local authorities and practitioners working with families including:
Reducing unintentional injuries in and around the home among children under 5 years sets out 3 action areas that aim to reduce the numbers of children injured and killed and describes 4 steps local partnerships can take to build robust injury prevention strategies.
Healthy Start is a UK-wide government scheme, embedded within the Healthy Child Programme, to improve the health of low-income pregnant women and families on benefits and tax credits.
Healthy Start provides a great opportunity for health professionals and others working with pregnant women and families to offer encouragement, information and advice on issues such as healthy eating, breastfeeding and vitamins.
Vouchers can be used to help families on a low-income buy some basic foods, such as milk and fresh or frozen fruit.
For the first 6 months of your baby’s life the safest place for them to sleep is in a cot in the same room as the person looking after them, for all sleeps.
Sadly, every year a small number of babies die suddenly and unexpectedly in their sleep. Sometimes a cause is found, such as an underlying health condition, but often there’s no obvious reason.
You may hear the term sudden infant death syndrome (SIDS) which used to be called cot death.
SIDS happens most often during sleep at any time, day or night. Doctors don’t yet know what causes it but it’s most likely to happen in the first 6 months. Babies born early and underweight, and twins or multiple babies are more
at risk.
What increases the risk of SIDS?
SIDS is at increased risk of happening if you:
SIDS is at increased risk of happening if your baby:
Breastfeeding your baby reduces the risks of SIDS
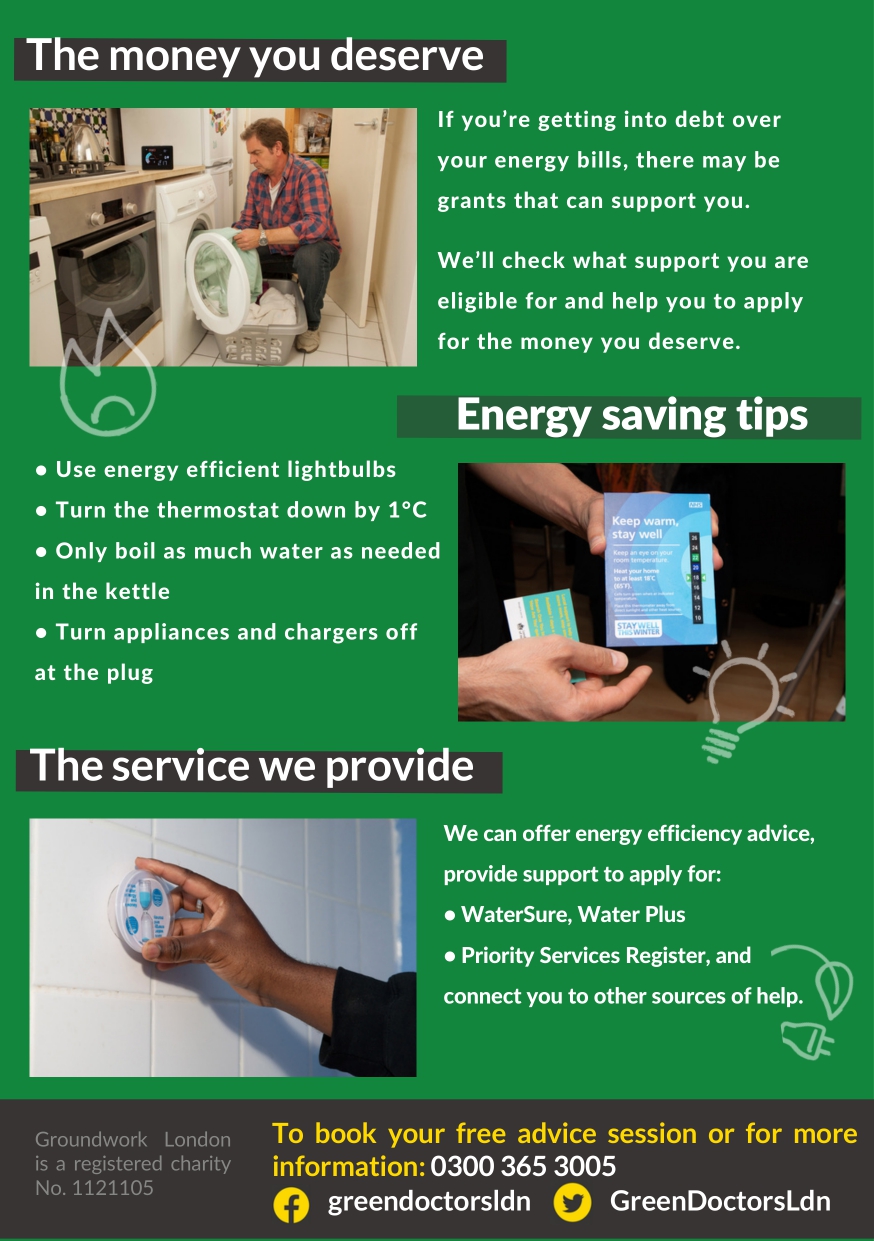
Energy saving advice from Energy Saving Trust
Find out more about how to fix damp and condensation here


Being homeless can mean more than living on the streets. You can be homeless even if you have a roof over your head. For example:
The earlier you can let us know about your housing problem, the more we can do. We cannot offer council housing to most people. So you may have to consider another option when looking for a new home.
If you find yourself homeless today and your enquiry is urgent, you can speak with a housing advice officer on: 0208 424 1093 (lines open 9am-5pm Monday to Friday.
For emergencies outside these hours including weekends, calls will be diverted to the Emergency Social Services.
High blood pressure can often be prevented or reduced by eating healthily, maintaining a healthy weight, taking regular exercise, drinking alcohol in moderation and not smoking.
The Eatwell Guide highlights the different types of food that make up our diet, and shows the proportions we should eat them in to have a well-balanced and healthy diet.
Salt raises your blood pressure. The more salt you eat, the higher your blood pressure. Aim to eat less than 6g (0.2oz) of salt a day, which is about a teaspoonful.
Find out how to cut down on salt
Eating a low-fat diet that includes lots of fibre, such as wholegrain rice, bread and pasta, and plenty of fruit and vegetables also helps lower blood pressure.
Having too much salt can cause high blood pressure.
If you’ve had a recent blood pressure test, you can find out what the reading means.
Check your blood pressure reading
If you are over 40, you can have a blood pressure reading as part of an
NHS Health Check, which is offered to adults in England aged 40 to 74 every 5 years.
Adults should have no more than 6g of salt a day (around 1 level teaspoon).This includes the salt that’s already in our food and the salt added during and after cooking.Maximum recommended salt intake
Babies should not have much salt, because their kidneys are not fully developed and cannot process it.
Tips to reduce your salt intake
Do
Don’t
NHS Healthier Families: Salt has more tips and information on foods that are high in salt
NHS Healthier Families: Recipes has healthy recipes you can try at home
Understanding food labels can help you choose foods that are low in salt
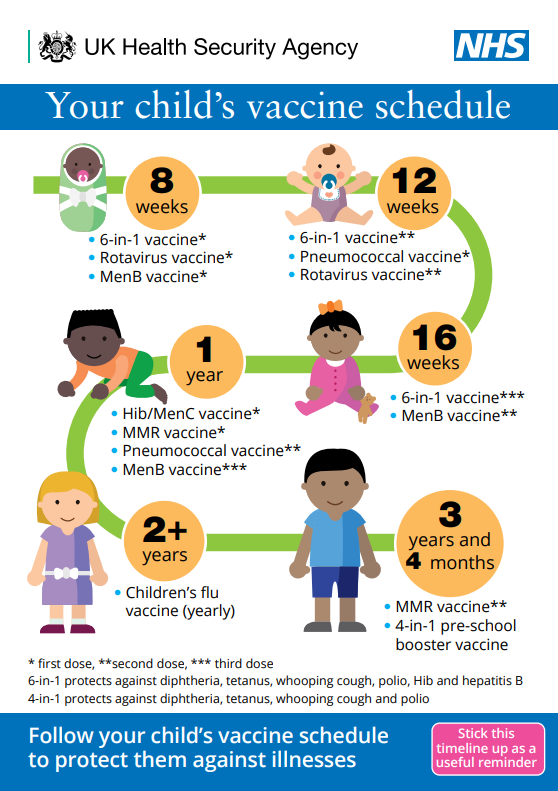
Vaccination is the most important thing we can do to protect ourselves and our children against ill health. They prevent millions of deaths worldwide every year. Since vaccines were introduced in the UK, diseases like smallpox, polio and tetanus that used to kill or disable millions of people are either gone or are now very rarely seen.
Other diseases like measles and diphtheria have reduced to a very low number of cases each year since vaccines were introduced. These cases are often related to travel. However, if people stop having vaccines, it’s possible for infectious diseases to quickly spread again.
Further information can be found here
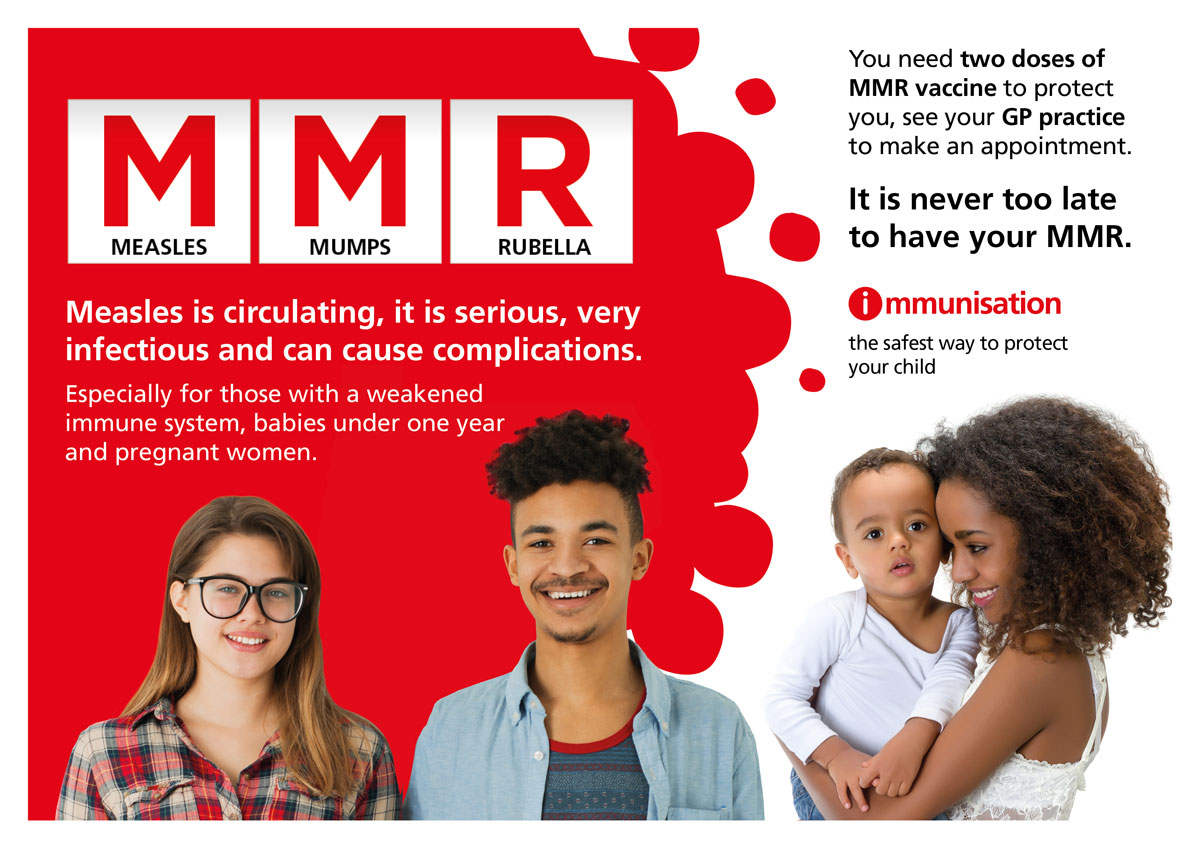


UKHSA and the NHS have launched a national campaign to support efforts to increase uptake of childhood immunisations among 0–5-year-olds and highlight the serious risk childhood diseases can pose if children aren’t vaccinated. In response to the recent rise in measles cases, the national campaign will run until mid-April 2024.
You are encouraged to:
Key messages
Further information can be found here

A learning disability affects the way a person learns new things throughout their life.
A learning disability is different for everyone. No two people are the same.
A person with a learning disability might have some difficulty:
Doctors and other health workers might be able to tell if a person has a learning disability when they are very young. But some people get a diagnosis later in their lives. This can be when they are adults.
If you are diagnosed with a learning disability, you might be referred to other health professionals to get the support you need.
A profound and multiple learning disability (PMLD) is when a person has a severe learning disability and other disabilities that significantly affect their ability to communicate and be independent.
Someone with a profound and multiple learning disability might have difficulties seeing, hearing, speaking and moving. They may have complicated health and social care needs due to these or other conditions.
People with a profound and multiple learning disability need support to help them with some areas of their life, such as eating, washing or personal care.
Lots of people with a profound and multiple learning disability can still be involved in decisions about themselves, do things they enjoy and be independent.People with profound and multiple learning disabilities (PMLD) are, like everyone else, unique individuals.
Some people who struggle with talking might be able to use other ways of communication, like sign language, Signalong, Makaton, or digital systems like picture exchange communication systems (PECS).
Different Learning disabilities explained on Mencap Page
Dedicated to ensuring all women and families impacted by perinatal mental health problems have access to high-quality, compassionate care and support. We bring the maternal mental health community together and make change happen by combining the power of real-life experience with clinical and professional expertise.
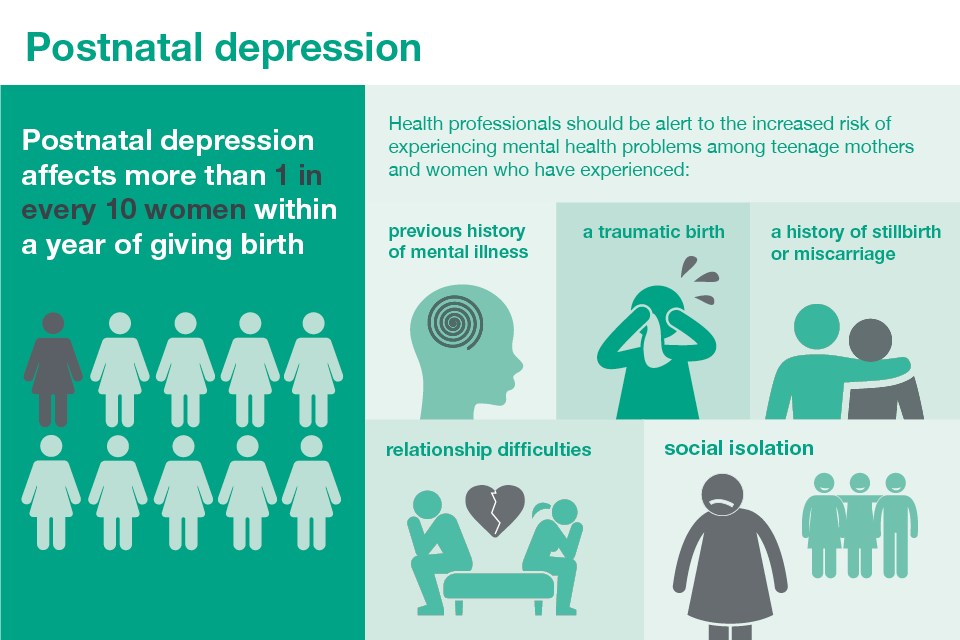
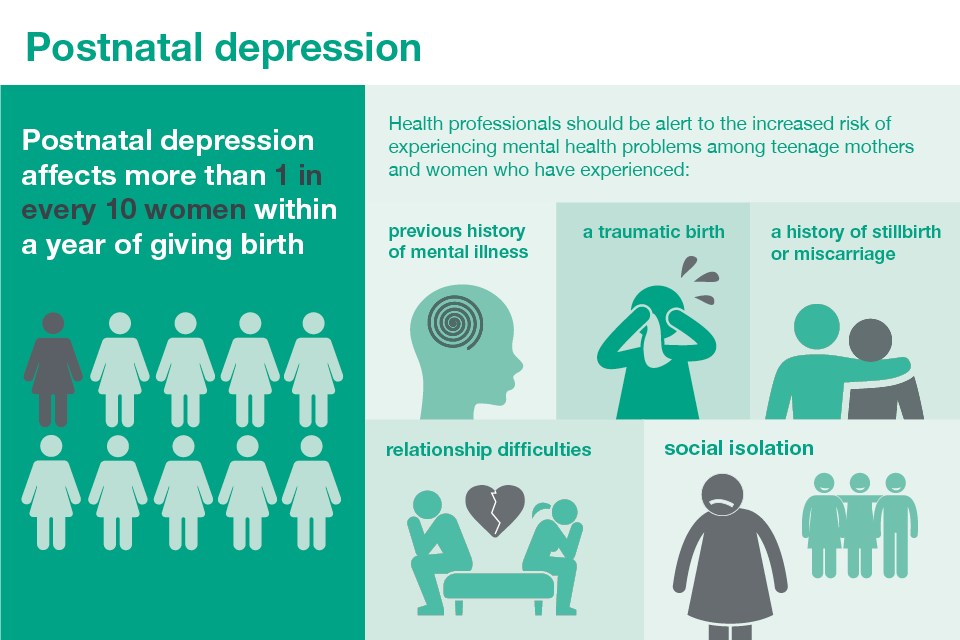
Postnatal depression is a type of depression that many parents experience after having a baby.
It’s a common problem, affecting more than 1 in every 10 women within a year of giving birth. It can also affect fathers and partners.
It’s important to get help as soon as possible if you think you might be depressed, as your symptoms could last for months or get worse and have a significant impact on you, your baby and your family.
With the right support most people make a full recovery.
Depression in pregnancy (antenatal depression) is also common, affecting more than 1 in 10 women.
Other mental health symptoms that can occur during or after your pregnancy include anxiety, panic attacks and psychosis.
Menopause is when your periods stop due to lower hormone levels. It usually affects women between the ages of 45 and 55, but it can happen earlier.
It affects anyone who has periods.
Menopause can happen naturally, or for reasons such as surgery to remove the ovaries (oophorectomy) or the uterus (hysterectomy), cancer treatments like chemotherapy, or a genetic reason. Sometimes the reason is unknown.
Perimenopause is when you have symptoms of menopause but your periods have not stopped. Perimenopause ends and you reach menopause when you have not had a period for 12 months.
Menopause and perimenopause can cause symptoms like anxiety, mood swings, brain fog, hot flushes and irregular periods. These symptoms can start years before your periods stop and carry on afterwards.
Menopause and perimenopause symptoms can have a big impact on your life, including relationships and work.
There are things you can do to help with symptoms. There are also medicines that can replace the missing hormones and help relieve your symptoms.
Lifestyle changes to help menopause and perimenopause:
Eating well, exercising and looking after your mental wellbeing can help with symptoms during perimenopause and menopause.
It can also help you keep as well as possible in the future.
The “male menopause” (sometimes called the andropause) is an unhelpful term sometimes used in the media.
This label is misleading because it suggests the symptoms are the result of a sudden drop in testosterone in middle age, similar to what occurs in the female menopause. This is not true.
Although testosterone levels fall as men age, the decline is steady at about 1% a year from around the age of 30 to 40, and this is unlikely to cause any problems in itself.
A testosterone deficiency that develops later in life, also known as late-onset hypogonadism, can sometimes be responsible for these symptoms, but in many cases the symptoms are nothing to do with hormones.
Some men develop depression, loss of sex drive, erectile dysfunction, and other physical and emotional symptoms when they reach their late 40s to early 50s.
Other symptoms common in men this age are:
A conversation starter tool to help you engage with friends, family, neighbours or those you support in your community or workplace about good mental health, wellbeing and financial worries.
If you’re living with a mental health problem, or supporting someone who is, having access to the right information is vital.
Mind in Harrow provides mental health support locally. Find out more about them
here


Neurodiversity refers to the different ways a person’s brain processes information.
Being neurodiverse does not correlate with low intelligence; many people with neuro differences are highly intelligent.
People who are neurodiverse often think about and see the world differently, making them a huge asset to any team that wants to improve how they do things and deliver excellent patient care or services.
You may have heard of many of these types of neurodiversity.
There are a number of other examples of how brains can process information differently.
Some people consider these to be part of the ‘neurodiversity’ umbrella and others like to keep them separate – there’s no right or wrong answer.
Oral and dental diseases are widely prevalent, and whilst oral health has improved in recent decades, most people are at risk of developing some oral disease during their lifetime. The most common diseases are dental caries and periodontal diseases, with oral cancer being the most serious, and tooth wear an increasing concern. The impact of oral disease (most notably dental caries) includes pain, days lost from work and school, and adversely affects
people’s quality of life.
More information and support can be found on the Oral Health Foundation website here.
Oral health assessment tool can be found here. Guidance from nice.org.uk
Dental Factsheets can be found here.
Public health are supporting the annual national campaign
National Smile Month which takes place between the 13 May and 13 June 2024 led by the Oral Health Foundation to raise awareness about the importance of good oral health.
The Harrow oral health promoters will be running various activities throughout the month.
Go to the News section to see the various activities that you can get involved with.

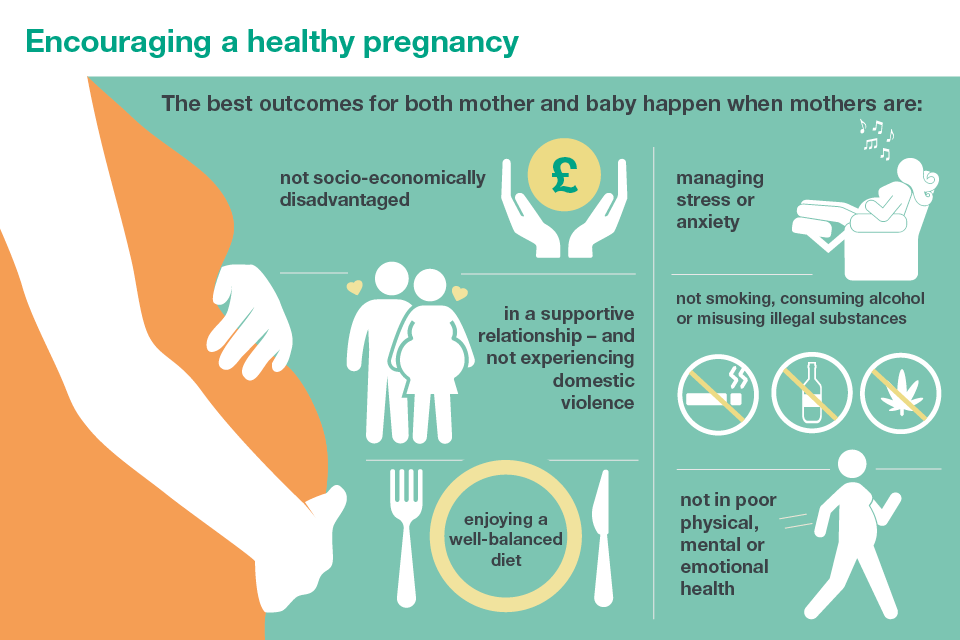
A healthy pregnancy and early years are important to the health of the developing baby. There is a growing body of evidence and research on neurological development, epigenetics and the impact of stress, anxiety and adverse experiences in pregnancy and the first years of life. This reiterates the importance of prevention, support for parents and early intervention.
Pregnancy and the early years provide an ideal opportunity for public health practitioners and other professional groups to advise and support parents on a range of issues including:
The Baby Plus You project is in collaboration with Central and North West London Perinatal Mental Health Services. The team is here to explain the referral process and answer any questions you have about Perinatal Mental Health services in Brent and Harrow.
Health before and during pregnancy is vital. A healthy woman is more likely to give birth to a healthy baby. Health professionals should support women (and their partners) to adopt positive health behaviours and reduce risk factors. Pre-conceptual care includes ensuring full immunisation status, advice on vitamins, and folic acid and advice on alcohol and tobacco and on nutrition.
A number of resources have been developed to help in planning and preparation for pregnancy, to improve outcomes for mothers and babies including making the case for preconception care, a report for local maternity systems and their wider systems partners.
The report is accompanied by these additional resources:
Between pregnancies, advice on family spacing, contraception services is important. Researchers of The prevalence of unplanned pregnancy and associated factors in Britain: findings from the third national survey of sexual attitudes and lifestyle identified that 45% of pregnancies in the UK are unplanned or associated with feelings of ambivalence. Pregnancies in young, single women are most likely to be unplanned.
STFYAYB provides information about the screening tests offered during and after pregnancy.
The information is available in 12 other languages: Arabic, Bengali, Chinese, French, Latvian, Lithuanian, Polish, Portuguese, Punjabi, Romanian, Somali and Urdu.
In this publication, the terms ‘woman’ and ‘women’ to refer to anyone able to become pregnant, including trans men. Trans men who are pregnant should be offered the same antenatal and newborn screening tests as other pregnant individuals.
These 8 easy read guides explain the screening tests offered during and after pregnancy for people with learning disabilities.
Depression in pregnancy (antenatal depression) is also common, affecting more than 1 in 10 women.
Other mental health symptoms that can occur during or after your pregnancy include anxiety, panic attacks and psychosis.
Postnatal depression
Postnatal depression is a type of depression that many parents experience after having a baby.
It’s a common problem, affecting more than 1 in every 10 women within a year of giving birth. It can also affect fathers and partners.
It’s important to get help as soon as possible if you think you might be depressed, as your symptoms could last for months or get worse and have a significant impact on you, your baby and your family.
With the right support most people make a full recovery.
Symptoms of a miscarriage
The main sign of a miscarriage is vaginal bleeding, which may be followed by cramping and pain in your lower abdomen.
If you have vaginal bleeding, contact a GP or your midwife.
Most GPs can refer you to an early pregnancy unit at your local hospital straight away if necessary.
You may be referred to a maternity ward if your pregnancy is at a later stage.
But bear in mind that light vaginal bleeding is relatively common during the first trimester (first 3 months) of pregnancy and does not necessarily mean you’re having a miscarriage.
Causes of a miscarriage
Chromosomes are genetic “building blocks” that guide the development of a baby.
If a baby has too many or not enough chromosomes, it will not develop properly.
In most cases, a miscarriage is a one-off event and most people go on to have a successful pregnancy in the future.
Preventing a miscarriage
The majority of miscarriages cannot be prevented.
But there are some things you can do to reduce the risk of a miscarriage.
Avoid smoking, drinking alcohol and using drugs while pregnant.
Being a healthy weight before getting pregnant, eating a healthy diet and reducing your risk of infection can also help.
After a miscarriage
A miscarriage can be an emotionally and physically draining experience.
You may have feelings of guilt, shock and anger.
Advice and support are available at this time from hospital counselling services and charity groups.
You may also find it beneficial to have a memorial for the baby you lost.
You can try for another baby as soon as your symptoms have settled and you’re emotionally and physically ready.
It’s important to remember that most miscarriages are a one-off and are followed by a healthy pregnancy.
Support groups
Sexual health clinics offer a range of services, including:
Sexual health clinics may also be called genitourinary medicine (GUM) or sexual and reproductive health (SRH) services. Not all clinics offer every service.
Check with the individual clinic to see what’s available.
Anybody can go to a sexual health clinic, no matter what their age. Some clinics hold sessions for specific groups of people, including young people, gay men and lesbians.
You may need to make an appointment at some clinics, while others offer “drop-in” sessions, where you can turn up without an appointment.
Appropriate arrangements should be in place so people with special needs can access sexual health services – for example, providing access to interpreters.
There should also be clinic facilities for people with physical disabilities, learning disabilities, people who’ve been sexually assaulted, sex workers and those who misuse substances.
All services are free and completely confidential, and all tests are optional.
Sexual health clinics can offer testing for STIs, such as:
Depending on which STIs you’re tested for, tests may include:
Smoking is the single greatest preventable cause of death in the world today. There are more than one billion smokers worldwide – that’s one-quarter of all adults – and it’s killing up to half the people who smoke.